|
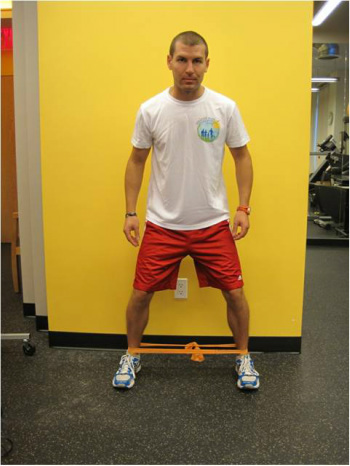
This is a follow up to my previous post Patellofemoral Pain Syndrome: What Is It? For the purposes of keeping this discussion on the shorter side I am going to skip the smaller subgroup of people who fall into the category of actual structural factors like a shallow patellar groove or bony abnormalities and focus on the majority of people who have functional deficits that can change with treatment. In most cases, the knee joint itself is usually healthy and absent any major issues but is sensitive and irritated as a result of deficits elsewhere. Upon examination, these deficits most commonly show up in the hip and/or the ankle. There are occasions where the lumbopelvic complex can play a significant role as well but not as frequently. For these reasons alone it is highly recommended to consult with a physical therapist who will perform a thorough physical exam to decipher which factors are the probable culprits causing the patellofemoral pain. Going back to 1976, Nicholas et al shed some light on this issue and found that proximal thigh muscle weakness was strongly associated with a variety of lower extremity conditions, particularly with patellofemoral pain. (1) More recently, Peters and Tyson performed a systematic review of the literature addressing proximal (read: hip) interventions and their effectiveness in resolving patellofemoral pain. Based on their review, there is very good evidence suggesting that proximal exercises is an appropriate and effective treatment, especially early on. (2) If you are wondering why this is the case, think of the hip as the foundation of your leg. Weak foundations of any structure leads to all kinds of problems and the same can be said of the hip. By strengthening the muscles of the hip and thigh you provide a solid foundation for the joints below, particularly the knee, to function as they were designed to. Another way to say that is strong hip and thigh muscles are able to control the mechanics of the knee more appropriately which can eliminate whatever was irritating the patellofemoral joint. Another driving factor can be below the knee at the ankle joint. The foot can as well but that's another topic for another day. To illustrate my point I've attached a video courtesy of Chris Johnson: As you can see, mobility and range of motion issues at the ankle can have a dramatic effect on knee positioning and mechanics. Imagine if that is what your knee is doing every time you squat, negotiate stairs or get out of your car. My knee(s) (patellofemoral joint) would be pretty cranky too! Last time I checked, the knee is supposed to flex forward and back more than rotate in. It doesn't take a rocket scientist to realize that this situation would completely change the forces and stresses applied through the patellofemoral joint potentially resulting in knee pain. Since I did not work with this individual it is unclear whether the ankle range of motion limitation is due to a loss of joint mobility, calf tightness or both. Again, this is why it is highly recommended to consult with a physical therapist who can figure out the main factors. Either way, by addressing the ankle through mobilizations and/or flexibility work, there is a high probability of resolving issues further up the chain like patellofemoral pain. At this point you might be saying "well that's great information but what can I actually do about it, Greg?" The following is by no means an exhaustive program but a good starting point for patellofemoral pain: Hip (Proximal) Strength
Ankle Mobility There are many good techniques to improve ankle dorsiflexion but this is my go to for two reasons: 1) It works, and 2) You don't necessarily need the compression wrap for it to be effective. For some other ideas and if you have access to wraps or bands, Mike Reinold put together a bunch of them in his aptly titled article Ankle Mobility Exercises To Improve Dorsiflexion. Calf Flexibility Calf Stretch Steps and stairs make for great calf stretching. In either case, your forefoot is placed on the edge with a slight toe in of about 5 degrees. If your heel is touching the floor, keep your leg straight and lean forward until you feel a strong stretch. If you are using a stair, allow your heel to drop until the same strong stretch is felt. Hold for 60-90 seconds and repeat 3-5 times. If you've been experiencing anterior knee pain or have even been diagnosed with Patellofemoral Pain Syndrome, these exercises may provide with some relief but consider consulting with a physical therapist who can fine tune your treatment. References: 1. James A. Nicholas, M.D., Alan Marc Strizak, M.D., George Veras, M.B.A., M.P.A. A study of thigh muscle weakness in different pathological states of the lower extremity. American Journal of Sports Medicine. December 1976, vol. 4, no. 6, 241-248. 2. JS Peters, NL Tyson. Proximal exercises are effective in treating patellofemoral pain syndrome: a systematic review. International Journal of Sports Physical Therapy. 2013 Oct; 8(5): 689-700. Knowledge = Power; Share the Power:
0 Comments
 Recently, I've been asked a few times about Patellofemoral Pain Syndrome (PFPS) as well as a few clients walk into my office with complaints of knee pain so I thought I'd put together some information to try to clarify some of the issues related to this common ailment. A quick Google search of 'Patellofemoral Pain Syndrome' provides you with almost 350,000 results and after this post, you'll be able to add another one to that list. Try many of the other iterations like PFPS, patellofemoral pain, patellofemoral syndrome, runner's knee, chondromalacia patella, movie-goers knee, etc. and you'll come up with thousands more. So what does this all mean? Well it means there is a ton of information (and misinformation) about one of, if not, the most common knee injuries to plague athletes, weekend warriors, office workers, young, old...just about anyone. The first goal is to define what it is. The simple version is pain around and/or behind the kneecap (patella) as it articulates or touches the femur. That sounds pretty straightforward but it can present itself in a variety of ways which is why you will find so many definitions/results with a Google search and among healthcare practitioners. It is also part of the reason why it has been given the vague designation of a 'syndrome'. The truth of the matter is nobody knows exactly what causes it or what is happening at the patellofemoral joint when PFPS shows up to the party. All we know is that the end result is pain. Since there is no consensus on what is actually happening, that makes finding a solution more challenging than say a broken bone or muscle strain. Add other knee injuries that can be confused with PFPS like iliotibial band syndrome (ITBS, yet another syndrome and another post), patellar tendonitis and bursitis and one can see how a 'simple' definition can become a complicated issue to diagnose and resolve. Though quite varied from person to person, there are some hallmark symptoms, however, that can help narrow down the differential diagnosis. These commonly include, but are not limited to, pain with squatting, ascending/descending stairs, running and prolonged sitting. Sometimes joint effusion or swelling will be present but again, this is quite variable also. Granted, these are common complaints among other knee injuries as well so PFPS often becomes a diagnosis of exclusion due to signs, tests and subjective complaints that can help distinguish between issues like meniscus pathology, tendonitis, bursitis, ITBS, etc. Now this is where physical therapists make the 'big bucks' (I can dream, right?). It is nice to have someone walk into my office with cookie cutter complaints so that the solution is easy but honestly, that situation doesn't happen very often. Instead, I am able to use my training and knowledge in anatomy, kinesiology and biomechanics, muscle physiology, neuroscience and psychology to assess the incredibly dynamic system that is the human body and brain to formulate a conclusion as to why someone is experiencing pain, in this case patellofemoral pain. Through careful observation, specific tests and measures, and most importantly, listening to my clients, I can deduce the driving factors of someone's patellofemoral pain and customize a plan to resolve his/her pain and limitations. Quite often, there are multiple factors involved and it is my job to determine the best way to address them and sequence the plan to get my clients back to moving better, feeling better and living better. Stay tuned for my next post to learn about some of the ways patellofemoral pain syndrome can be resolved. Knowledge = Power; Share the Power: |
Dr. Greg Cecere
Your personal physical therapist, movement educator and knowledge dispenser. Newsletter Sign Up
Enter your name and email to get Momentum PT's Movement Manual delivered straight to your inbox! It's your free monthly newsletter and guide to moving better, feeling better and living better! Archives
April 2017
Categories
All
Disclaimer:
The contents of this blog is meant for educational purposes only. Momentum Physical Therapy of New Paltz and Dr. Greg Cecere are not responsible for any harm or injury that may occur due to any information on this blog as it is by no means a substitute for a thorough evaluation by a medical professional. |
|
Momentum Physical Therapy of New Paltz, PLLC. Copyright © 2013-2024. All Rights Reserved.
Disclaimer: The contents of this site is meant for educational purposes only and utilization of any of the material is a personal choice. Momentum Physical Therapy of New Paltz and Dr. Greg Cecere are not responsible for any harm or injury that may occur due to those choices. This site is by no means a substitute for a thorough evaluation and guidance by a licensed medical professional.
|

 RSS Feed
RSS Feed
